What is a polyp?
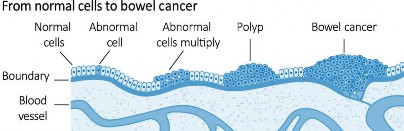
A bowel polyp is an abnormal fleshy growth extending from the inner wall of the large bowel (colon and rectum). About half of all Australians will develop a bowel polyp during their lifetime, but most of these remain undetected. If polyps are left untreated for many years, some can develop into bowel cancer. Polyps vary in type, shape, size, location and number:
- Type of polyps: Polyps are divided into three main types: adenomatous polyps (also known as adenomas), hyperplastic polyps and sessile serrated lesions (SSLs). Adenomas and SSLs can develop into bowel cancer in a process that takes many years. Hyperplastic polyps do not develop into cancer. Adenomas and SSLs may occur in patients with rare genetic syndromes.
- Shape of polyps: The word ‘sessile’ describes a flat polyp that is only slightly raised above the surrounding normal bowel lining. Other polyps appear as a fleshy cap, raised on a stalk, like a mushroom. These polyps are called ‘pedunculated’.
- Size of polyps: Most polyps are small, less than 1 cm. Some polyps, however, can grow to be several centimetres wide.
- Location of polyps: Polyps are also described by their position within the large bowel.
- Number of polyps: The number of polyps found during a colonoscopy is written in the report, either as a total number or as the number of polyps in a particular area in the bowel.
How are polyps related to bowel cancer?
Bowel cancer is the most common internal cancer, with 13,000 new cases each year. Each week, about 80 Australians die from bowel cancer. It is the second most common cause of death from cancer in Australia.
Polyps are usually non-cancerous. However, some can develop into bowel cancer in the future.
Polyps and early bowel cancer can be found through a simple two-minute ‘poo test’ (called a faecal occult blood
Information about
Bowel Polyps

Magic mine | shutterstock.com
test – ‘FOBT’) and by colonoscopy. These tests are the best way of preventing bowel cancer because polyps can be removed early, before they can turn into cancer, or by
catching bowel cancer at an early, treatable stage.
Bigger polyps and adenomas have a greater risk of developing into cancer. At the time of colonoscopy, there is no way of knowing which polyps have this potential. So, where possible, all polyps are removed.

SciePro | shutterstock.com
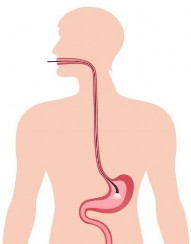
Removal of a polyp (polypectomy) is done using a small wire loop, like a lasso, which is passed over the top of the polyp
and then closed at its base to cut the polyp off.
Am I cured?
An individual polyp is usually cured by polypectomy, which also removes any potential cancer risk from that polyp.
Once removed, the polyp is sent to a laboratory to ensure that it is benign (does not contain cancer). Rarely, cancer is found within the polyp, and surgery may then be needed to make sure all the cancer is removed from the bowel.
The importance of a polyp does not end with its removal. A person who has had a polyp or cancer in the past is at greater risk of developing polyps or cancer in the future.
How often do I need to be checked?
Depending on the type, size and number of bowel polyps that are removed, your doctor will advise about the need for future colonoscopies and when you should have them. The gap between colonoscopies may be shorter if your doctor wants to check that a polyp was completely
Bowel polyps often have no symptoms!
Risks for polyps include older age, family or personal history of bowel polyps or cancer, and blood in bowel motions.
Who is at risk of bowel cancer?
Both men and women are at risk of developing bowel cancer. In Australia, the lifetime risk of developing bowel cancer before the age of 75 years is about 1 in 19 for men and 1 in 28 for women. This is one of the highest rates of bowel cancer in the world. The risk is greater for people who:
-
are aged 50 years or older – risk increases with age
-
have a significant family history of bowel cancer
-
have had an inflammatory bowel disease, such as
Crohn’s disease or ulcerative colitis
-
have previously had certain types of polyps, called adenomas, in the bowel
-
have risky lifestyle factors, including smoking and weight above the healthy weight range
People at above-average risk of bowel cancer should talk to their doctor about their screening options.
removed or if the colonoscopy was incomplete. Some people with a strong family history of bowel cancer or many bowel polyps may also undergo more frequent follow-up.
Colonoscopy is the best way of finding polyps and the only way of removing them from the bowel. Nevertheless, no medical test is perfect, and occasionally polyps may be missed during your first colonoscopy.
What happens after polyp removal?
Polypectomy is safe and effective. There is a very small risk of bleeding from the place where the polyp was removed, and an even smaller risk of a small hole being made in the bowel wall (perforation). These conditions may require treatment in hospital. If you have significant bleeding from the bowel or prolonged or new abdominal discomfort after the procedure, you should seek medical attention.
What can I do to prevent polyps and bowel cancer in the future?
Being involved in the National Bowel Cancer Screening Program by using FOBTs when recommended is a good start. You should also try to have a healthy lifestyle, including not smoking, maintaining a healthy body weight, taking part in regular physical exercise and enjoying a nutritious diet.
If you have any questions or need advice, please talk to your doctor.
Acknowledgements
This resource was reviewed and updated by the following health professionals in 2022:
Dr Adam Haigh, Gastroenterology Advanced Trainee, Gold Coast University Hospital, Gold Coast QLD Australia
Dr Matthew Remedios, Senior Consultant Gastroenterologist, Royal Brisbane and Women’s Hospital, Brisbane QLD Australia
Requests and enquiries concerning reproduction and rights should be addressed to: Gastroenterological Society of Australia (GESA) Level 1, 517 Flinders Lane, Melbourne VIC 3000 | Phone: 1300 766 176 | email: gesa@gesa.org.au | Website: http://www.gesa.org.au
This document has been prepared by the Gastroenterological Society of Australia and every care has been taken in its development. The Gastroenterological Society of Australia and other compilers of this document do not accept any liability for any injury, loss or damage incurred by use of or reliance on the information. This work is copyright. You may download, display, print and reproduce this material in unaltered form only (retaining this notice) for your personal, non-commercial use or use within your organisation. Apart from any use as permitted under the Copyright Act 1968, all other rights are reserved. © 2022 Gastroenterological Society of Australia ABN 44 001 171 115.