COLONOSCOPY FACT SHEET
What is colonoscopy?
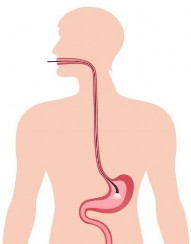
A colonoscopy (scope) is the examination of the lower gastrointestinal tract to diagnose, and in some cases, treat problems. This procedure involves passing a colonoscope – a long, thin flexible tube with a ‘video camera’ at the tip – through the rectum into the colon (large intestine, large bowel). It allows the doctor to inspect the colon and to perform specialised procedures such as taking biopsies for pathology and removal of polyps (abnormal growths which sometimes develop into cancer).
Why have a colonoscopy?
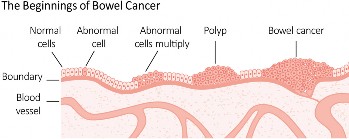
Colonoscopy can detect polyps, inflamed tissues and cancers, such as colorectal cancer. It can help doctors diagnose unexplained changes in bowel habits, abdominal pain, bleeding from the bowel and weight loss. In some individuals with a family history of colon cancer, it may be an appropriate test and may even help to prevent colon cancer.
How do I prepare for colonoscopy?
For a colonoscopy to be successful, it is essential to empty the bowel thoroughly of all waste material. This is done by taking a bowel preparation that will cause diarrhoea (see below). If the colon is not clean, the doctor may not be able to examine the bowel lining properly, and you may have to return for another procedure.
A complete bowel preparation consists of:
-
Modifying your diet
This may involve a special diet for several days prior to the colonoscopy. It is generally advised that you avoid foods containing seeds and grains for several days before the test because they can block the suction channel of the instrument.
-
Taking a bowel preparation
There are several bowel preparations (laxatives that cause diarrhoea and empty the colon). Depending on your medical condition, your doctor will recommend the right one for you.
A complete bowel preparation is essential for an accurate and safe colonoscopy. Please follow exactly the bowel preparation instructions.
-
Increasing your fluid intake
Specific instructions will be given to you by your doctor.
You should inform the doctor of all medical conditions and any medications, vitamins or supplements taken regularly. Iron supplements are generally stopped a week before the procedure.
How is colonoscopy performed?
Sedation
For the procedure deep sedation is usually given. You may be vaguely aware of what is going on in the room, but generally you will have little recollection of the procedure. The doctor and
medical staff will monitor your breathing, pulse and blood pressure during the procedure and will make you comfortable.
A colonoscopy usually takes between 20 and 45 minutes.
Examination of the bowel
Once you are sedated and lying on your left side, the doctor passes the instrument through the anus and into the colon. A small camera in the end of the scope transmits a video image to a monitor, allowing the doctor to examine the intestinal lining.
Once the scope has reached the point where the small intestine joins the colon, it is withdrawn carefully and the lining of the colon is examined again.
Removal of polyps and biopsy
A polyp is a small tissue growth on the bowel wall. They are common and are usually harmless, but a small proportion of them will develop into cancer. Removing them is an effective way of preventing cancer.
Small tissue samples (biopsies) of the colon may also be taken for examination under a microscope for signs of disease.
Following the procedure you will remain in the recovery area for an hour or two until the sedation wears off. You will usually be given something to eat and drink once you are fully awake.
You may feel a little bloated due to the air that is used to inflate the colon to allow adequate inspection of the lining. It generally passes within an hour or two.
Rarely you may pass a small amount of blood. This is often due to the samples that have been taken and should settle.
Because of the sedation given during the procedure, it is very important that you do not drive a car, travel on public transport alone, operate machinery, sign legal documents or drink alcohol on the day of the colonoscopy. It is strongly advised that a friend or relative takes you home and stays with you.
Full recovery is expected by the next day. It is important to read your discharge instructions carefully.
Are there any risks or side effects?
Although complications can occur, they are rare when the procedure is performed by doctors who are specially trained in colonoscopy.
In Australia, very few people experience serious side effects from colonoscopy and polypectomy (polyp removal).
The chance of complications depends on the exact procedure that is being performed and other factors including your general health.
Very rarely (one in 1,000 cases), the bowel lining may be torn; if this occurs you will be admitted to hospital for an operation to repair the lining.
Occasionally, people may react to the bowel preparation medication and experience headaches or vomiting.
Reactions to the medications used for sedation are also possible, but again rare.
In a few cases, if the colonoscopy is not successfully completed it may need to be repeated.
If you have any of the following symptoms up to 14 days after the colonoscopy you should contact the hospital or your doctor’s rooms immediately:
Severe abdominal pain
Black, tarry poo
Persistent bleeding from the anus
Fever
Other symptoms that cause you concern.
How accurate is a colonoscopy?
Colonoscopy provides the most accurate examination of the colon. However, no test is perfect and there is a small risk that an abnormality may not be detected.
A colonoscopy can miss small polyps in the bowel in 2 to 8 per cent of cases. For bigger abnormalities such as cancer, the chance is much less, but still present. For these reasons, it is recommended that all patients over the age of 50, and those with a family history of colorectal cancer, perform a faecal occult blood (FOB) test every one to two years and/or participate in the National Bowel Cancer Screening Program. The FOB test kits are available from your chemist or local doctor.
Sterilisation of the instruments
In accordance with GESA guidelines, the colonoscope and all instruments should be completely cleaned between each patient so that there should be no risk of transmission of serious diseases such as HIV and hepatitis B or C.
Who can I contact if I have any questions?
If you have any questions or need advice, please speak to your doctor before the procedure.
Important points
Colonoscopy is a procedure used to see inside the colon and rectum.
Prior to the procedure, use a bowel preparation kit to empty all solids from the gastrointestinal tract. Read the instructions carefully.
During colonoscopy light sedation is generally used to keep you comfortable.
The doctor will remove polyps and biopsy abnormal- looking tissue if found during the colonoscopy.
Driving is not permitted for 24 hours after a colonoscopy to allow the sedative time to wear off.
This document has been prepared by GESA and every care has been taken in its development. GESA and other compilers of this document do not accept any liability for any injury, loss
or damage incurred by use of or reliance on the information. This work is copyright. You may download, display, print and reproduce this material in unaltered form only (retaining this notice) for your personal, non-commercial use, or use within your organisation. Apart from any use as permitted under the Copyright Act 1968, all other rights are reserved.
Year of publication 2012 | Updated 2019 Gastroenterological Society of Australia
L1, 517 Flinders Lane, Melbourne VIC 3000 Australia
©2019 Gastroenterological Society of Australia ABN 44 001 171 115.
Requests and enquiries concerning reproduction and rights should be addressed to:
E-mail: gesa@gesa.org.au Website: http://www.gesa.org.au