This test is performed to investigate symptoms such as bleeding, pain, nausea and difficulty swallowing.
What is gastroscopy?
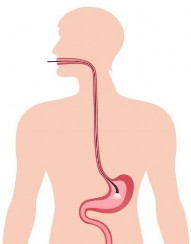
Gastroscopy is a test procedure done using an endoscope, which is a long, thin, flexible tube with a ‘video camera’ at the tip. This tube is passed through the mouth into the oesophagus (food pipe), stomach and first part of the small intestine. It allows the doctor to inspect these areas and perform other procedures, such as biopsies.
Why is gastroscopy done?
Gastroscopy is usually done to investigate symptoms of indigestion, belly pain, nausea, vomiting or difficulty swallowing. It is also the best test for finding the cause of bleeding in the upper gut.
Gastroscopy is more accurate than x-rays for finding inflammation, ulcers or tumours in the upper gastrointestinal tract. Biopsies (samples of tissue) can be taken to look for conditions such as infection, inflammation, coeliac disease or cancer.
Gastroscopy is also used to treat conditions of the upper gastrointestinal tract. Your doctor can pass small instruments through the endoscope to directly treat many abnormalities. This usually causes little or no discomfort. For example, your doctor might stretch a narrowed area, remove polyps (usually benign growths) or treat bleeding.
How do I prepare for gastroscopy?
An empty stomach is essential for a safe and accurate examination. You should have nothing to eat or drink, including water, for six hours before the gastroscopy. Your doctor will provide more specific details about this, depending on the time of day that your test is scheduled.
Tell your doctor in advance about any medications you take, particularly blood-thinning medications such as
Information about
Gastroscopy
(Upper Endoscopy)
Macrovector | shutterstock.com
aspirin products, clopidogrel (Plavix®), ticagrelor (Brilinta®), warfarin, rivaroxaban (Xarelto®), apixaban (Eliquis®) and dabigatran (Pradaxa®), as well as any diabetes medications or insulin.
You might need to adjust your usual dose
for the examination – this is particularly important if you have diabetes. You can keep taking most medications as usual. If you have any allergies to medications or any medical conditions, such as heart or lung disease, discuss these with your doctor.
How is gastroscopy performed?
Before the procedure, a light anaesthetic (sedative) is usually given – you will not usually receive a full general anaesthetic. You may be slightly aware of what is going on in the room, but most people don’t remember anything. The back of your throat may be sprayed with local anaesthetic to make it numb. A small mouthguard will be put between your teeth to stop you from biting the endoscope. If you have false teeth (dentures), they may be removed before the procedure.
The procedure takes about 15 to 30 minutes. Once you are sedated and lying in a comfortable position on your left side, the endoscope is passed through the mouth and then through the oesophagus, stomach and first part of the small intestine. The tube is about one centimetre in diameter and does not enter your windpipe, so it won’t interfere with your breathing. A small camera in the end of the endoscope transmits a video image to a monitor, allowing the doctor to carefully examine the lining of your upper gastrointestinal tract.
What happens after gastroscopy?
You will be monitored in the recovery area until most of the effects of the sedative have worn off. Your throat might be a little sore, and you might feel bloated because of the air introduced into your stomach by the endoscope during the test. You will be able to eat after you leave, unless your doctor instructs you otherwise.
Your doctor will usually briefly tell you your test results on the day of the procedure. A follow-up appointment may be made to discuss the test results more fully. The results of any biopsies will take several days.
Because of the sedative given, it is very important that you do not drive a car, travel on public transport alone, operate machinery, sign legal documents or drink alcohol for the rest of the day after the test. It is strongly advised that a friend or relative takes you home and stays with you.
Full recovery is expected by the next day. Discharge instructions should be carefully read and followed.
Are there any risks or side effects?
Complications are rare when the procedure is performed by doctors who are specially trained in gastroscopy. In Australia, very few people experience serious side effects from gastroscopy. The chance of complications depends on the exact type of procedure that you have and other factors, including your general health.
You may have a slightly sore throat after the procedure. Air may also be trapped in your stomach, causing you to feel bloated. If a biopsy has been taken or treatment performed, there may be minor bleeding. Very rarely, the
stomach lining may be torn, and if this happens, you will be admitted to hospital for an operation to repair it.
Reactions to the sedative are also possible but rare. After the procedure, there is a very small risk of developing a chest infection.
In a few cases, if the gastroscopy is not successfully completed, it may need to be repeated. If you have any of the following symptoms in the hours or days after the gastroscopy, you should contact the hospital or your doctor immediately:
- Fever
- Trouble swallowing
- Increasing throat, chest or abdominal pain
- Other symptoms that cause you to worry
Take-home points
- Gastroscopy is a procedure used to see inside the oesophagus (food pipe), stomach and first part of the small intestine
- An empty stomach is essential for a safe and accurate examination
- During gastroscopy, a light anaesthetic is often used to keep the patient comfortable
- The doctor will usually remove polyps and biopsy abnormal-looking tissue during the gastroscopy
- Driving is not permitted for 24 hours after gastroscopy to allow the sedative time to wear off
Who can I contact if I have any questions?
If you have any questions or need advice, please talk to your doctor before the procedure.
Acknowledgements
This resource was reviewed and updated by the following health professionals in 2022:
Dr Adam Haigh, Gastroenterology Advanced Trainee, Gold Coast University Hospital, Gold Coast QLD Australia
Dr Matthew Remedios, Senior Consultant Gastroenterologist, Royal Brisbane and Women’s Hospital, Brisbane QLD Australia
Requests and enquiries concerning reproduction and rights should be addressed to: Gastroenterological Society of Australia (GESA) Level 1, 517 Flinders Lane, Melbourne VIC 3000 | Phone: 1300 766 176 | email: gesa@gesa.org.au | Website: http://www.gesa.org.au
This document has been prepared by the Gastroenterological Society of Australia and every care has been taken in its development. The Gastroenterological Society of Australia and other compilers of this document do not accept any liability for any injury, loss or damage incurred by use of or reliance on the information. This work is copyright. You may download, display, print and reproduce this material in unaltered form only (retaining this notice) for your personal, non-commercial use or use within your organisation. Apart from any use as permitted under the Copyright Act 1968, all other rights are reserved. © 2022 Gastroenterological Society of Australia ABN 44 001 171 115.